According to the World Health Organization (WHO), pneumonia accounted for 14% of all deaths in children under five years old (about 740,180 kids total) in 2019. However, in the U.S., this number drops to fewer than 500 deaths in young children, thanks to vaccinations and medical care access.
What is Pneumonia?
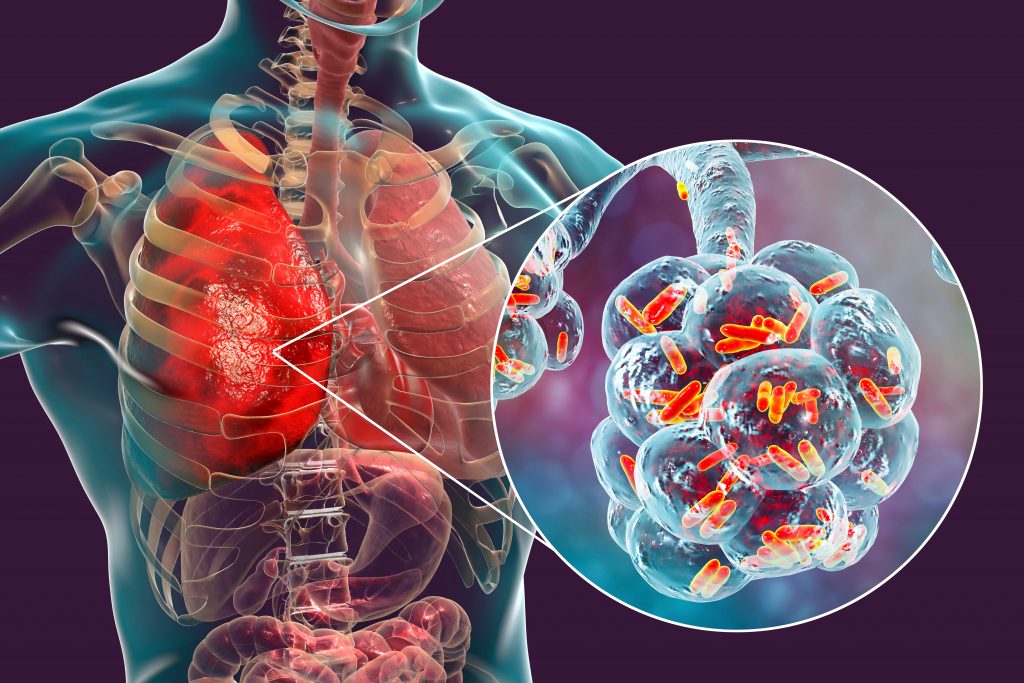
The Centers for Disease Control and Prevention (CDC) defines pneumonia as “an infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus.” Simply put, pneumonia is a lung infection that makes it difficult to breathe.
There are different types of pneumonia: community-acquired pneumonia, hospital-acquired pneumonia, walking pneumonia and aspiration pneumonia. Community-acquired is the most common and refers to getting sick from an everyday setting such as school or work. Hospital-acquired pneumonia happens when patients become sick during a hospitalization and tends to be more serious and resistant to treatment. Walking pneumonia is a milder form of the disease, which can feel like a lingering cold that won’t go away. Aspiration pneumonia is caused by accidental ingestion of food or liquid into the lungs.
Pneumonia can also be categorized by the cause of infection: bacterial, viral or fungal.
• Bacterial pneumonia is the most common cause of severe infection in both children and adults. Streptococcus pneumoniae (“pneumococcus”) as well as Haemophilus influenzae, Staphylococcus aureus and others are the most frequent bacteria that can lead to pneumonia.
• Viral pneumonia is very common and accounts for a large percentage of mild to moderate cases acquired in the community, especially in young children. Flu, COVID-19, respiratory syncytial virus (RSV) and adenovirus are common culprits for causing viral pneumonia.
• Fungal pneumonia is the least common form and is usually seen in those with weakened immune systems or who reside in certain geographical areas (not North Central Florida). Environmental molds and yeasts such as Histoplasma, Coccidioides (“Valley fever”), Cryptococcus and Aspergillus are often to blame for initiating this variation.

Who is at Risk?
While anyone can fall victim to pneumonia, some groups are more vulnerable than others. According to the National Heart, Lung and Blood Institute (NHLBI), young children, older adults, those with chronic illnesses (heart disease, diabetes, asthma, COPD), those who may be immune-compromised due to HIV, transplant or cancer treatment, smokers and heavy drinkers are at greatest risk for infection.
Is it a Cold or Something More?
While pneumonia can have some symptoms that overlap with the common cold, there are some symptoms that stand out.
• Bacterial pneumonia infections tend to have an acute onset (often at the end of a cold or flu) with a rapid progression of symptoms, such as a high fever with chills and sweats, productive cough (often thick, green or rust-colored) and chest pain that worsens with deep inhalations.
• Viral pneumonia tends to have a more gradual onset, often after a cold or flu. Fevers are often low to moderate temperature (though they may spike with a flu infection) with a dry or mildly productive cough. Viral pneumonia may also cause wheezing, diffuse body aches and occasional gastrointestinal symptoms (with a COVID or flu infection).
• Fungal pneumonia can either come on subacutely or chronically over a few weeks. Fungal pneumonia may or may not cause a fever, which tends to be low-grade if present. Any cough may be dry or produce a small amount of sputum. Other possible symptoms include night sweats, weight loss and a history of travel or exposure to environmental factors such as caves or bird droppings.
Prevention
Typical disease prevention tips such as frequent handwashing and covering coughs and sneezes as well as lifestyle factors such as adequate sleep and nutrition, stopping smoking and regular exercise will help prevent infection. In addition, routine vaccinations such as pneumonia vaccines, flu vaccine and COVID-19 can help prevent infections.
Healthy children are currently given a four-dose series of pneumonia vaccines in the first year of life. Children with certain medical conditions such as immune system disorders, chronic illnesses like heart disease, lung disease, or sickle cell disease, asplenia (absent or not functioning spleen), cochlear implants or cerebrospinal fluid (CSF) leaks may need additional prevention techniques.
Treatment
Depending on the type of infection, treatment may include antibiotics or supportive care for symptoms. It’s important to rest and drink plenty of fluids during the recovery period to expedite healing as well as finishing the entire course of antibiotics, even if symptoms subside.
While pneumonia can be serious, prompt recognition, prevention through vaccination and timely treatment make a full recovery the norm for most families. Schedule flu and pneumococcal vaccines to face the season armed with some protection, and see a doctor if symptoms persist.